Medical coding is an important part of healthcare administration as it ensures that medical procedures and diagnoses are documented accurately for billing and payment purposes.
A medical coder’s function is critical in sustaining a healthcare organization’s financial health and facilitating the right patient care records.
Mistakes in Medical Coding
The intricacy of the healthcare system and constant changes in coding standards make it a challenging field to fully comprehend.
Audits conducted by the government and private insurance companies have found shocking instances of fraudulent or abusive medical billing practices. You deserve to be compensated for the medical services you give, but it is critical that you avoid inappropriate billing practices in order to prevent difficulties and keep your practice thriving.
Importance of Medical Coding
- It ensures that healthcare practitioners are fairly compensated for the services they perform. Incorrect or missing codes can result in underpayment or delayed payments.
- Continuous errors can even impact your relationship with your patients.
- Accurate coding is required for statistical and research purposes, allowing healthcare professionals to analyze data and make sound judgments.
- Proper coding promotes effective communication among healthcare practitioners, insurers, and regulatory authorities.
Common Medical Coding Mistakes and Ways to Avoid Them
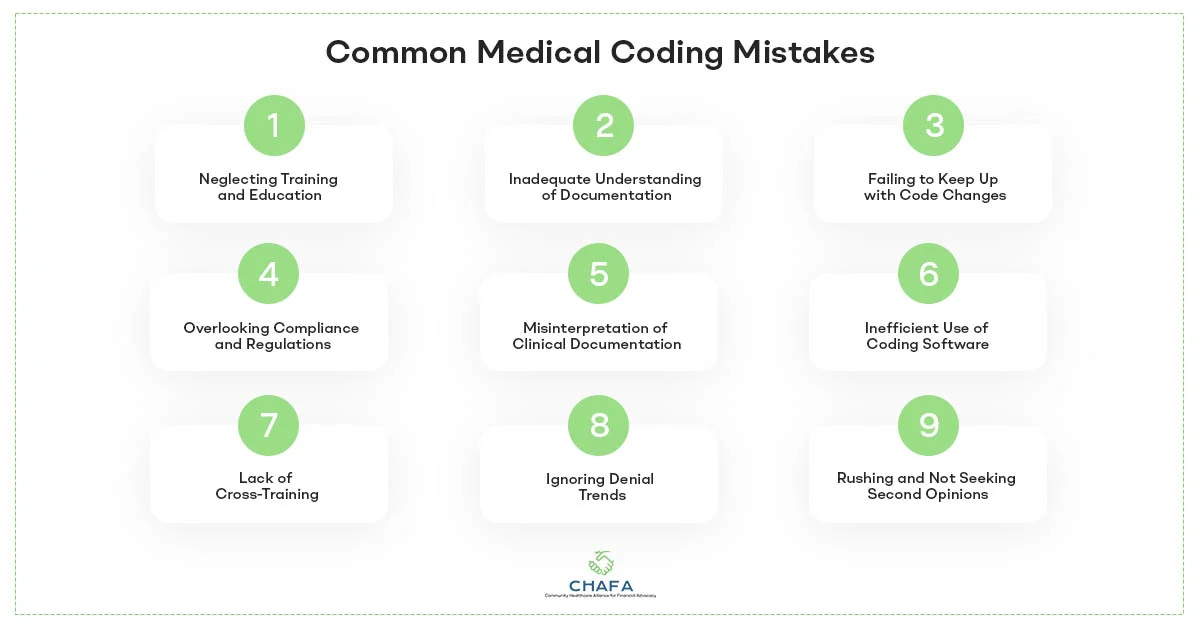
1) Neglecting Training and Education
The healthcare sector keeps evolving with improved procedures, technology, and laws introduced on a regular basis. Medical coders need to stay up to date on the most recent coding guidelines, regulations, and best practices. Failure to do so could result in coding mistakes, compliance concerns, and reimbursement delays.
Medical coders should invest time in continual training and education to prevent making this mistake. To keep current in their industry, professionals can attend workshops, webinars, and conferences. They can also pursue certifications such as Certified Professional Coder (CPC) or Certified Coding Specialist (CCS).
2) Inadequate Understanding of Documentation
The accuracy of medical coding is determined by the quality of clinical documentation. Using insufficient or ambiguous documentation is one of the most common mistakes medical coders make. If coders do not fully comprehend a patient’s condition, treatment, or procedures, they could write inaccurate codes, resulting in claim denials and revenue loss.
Medical coders ought to establish open lines of contact with healthcare providers to solve this issue. Regular meetings or inquiries could help in the resolution of any paperwork difficulties.
3) Failing to Keep Up with Code Changes
Medical coding is closely monitored, and code sets are changed on a regular basis to reflect changes in medical procedures, technology, and language. Medical coders who fail to keep up with these changes risk employing out-of-date codes, which can result in claim denials and compliance concerns.
To avoid making this error, medical coders ought to sign up for coding journals, newsletters, or websites that provide code change updates. They should also check coding rules produced by organizations such as the American Medical Association (AMA) and the Centres for Medicare and Medicaid Services (CMS) on a regular basis.
4) Overlooking Compliance and Regulations
Medical coders must follow healthcare rules at all times. Ignoring compliance requirements, such as those outlined in the Health Insurance Portability and Accountability Act (HIPAA) or the Office of Inspector General (OIG), can result in severe consequences, such as fines and legal action.
To avoid concerns with compliance, coders must be well-versed in these regulations and guarantee that they are followed consistently. This includes securing patient information, comprehending code bundling and unbundling requirements, and adhering to Correct Coding Initiative (CCI) modifications.
5) Misinterpretation of Clinical Documentation
Misinterpretation of clinical paperwork is another common error. Medical coders must be fluent in medical terminology and comprehend disease processes, surgical procedures, and therapies. Misinterpretations can result in incorrect coding, claim denials, and serious patient injury.
To reduce this possibility, medical coders should dedicate time to expanding their medical understanding. Continuous learning and communication with healthcare Advocacy experts can assist them in gaining a deeper grasp of clinical documentation, lowering the likelihood of misinterpretation.
6) Inefficient Use of Coding Software
Many medical coders rely on specialized coding software to make their jobs easier. However, inappropriate use of these technologies can result in problems. This could include failing to update software or failing to tailor software to the needs of the organization.
To prevent making this mistake, developers should receive extensive training in the use of coding software. Regular software updates and optimization are required to ensure accurate coding and effective operations.
7) Lack of Cross-Training
Medical coders can specialize in a certain area of coding, such as inpatient, outpatient, or surgery coding. Being too narrowly focused, on the other hand, can limit their abilities and adaptability. Medical coders who have not received cross-training may struggle to code accurately when confronted with issues outside their specialty.
Organizations should encourage cross-training among their coding teams to prevent this problem. Medical coders should have a basic awareness of several coding domains in order to adapt to changing situations and help their colleagues whenever necessary.
8) Ignoring Denial Trends
Claim denials can be a significant source of revenue loss for healthcare organizations. Ignoring denial trends and failing to address their root causes can lead to ongoing financial challenges.
Medical coders should analyze denial patterns regularly and collaborate with revenue cycle management teams to implement corrective actions. By identifying and resolving recurring issues, organizations can reduce denials and improve their revenue flow.
9) Rushing and Not Seeking Second Opinions
The urge to fulfill productivity goals can sometimes cause coders to speed through their work, increasing the likelihood of errors. In medical coding, quality should always take precedence over quantity.
Medical coding is a complicated process, and coders may come across situations with strange or confusing paperwork. In such cases, coders should seek a second perspective or confer with more experienced colleagues.
To avoid making these mistakes, medical coders should organize their time properly, allocating enough time to evaluate and code each case accurately. Additionally, promoting a collaborative and knowledge-sharing culture within the coding team can help coders manage difficult issues more efficiently and lower the likelihood of errors.
Conclusively, medical coding is an essential component of healthcare operations, having an impact on both financial performance and patient care. Avoiding frequent medical coding errors is critical for accurate documentation, regulatory compliance, and expedited revenue cycles. Medical coders can make a substantial contribution to the success of healthcare organizations and the well-being of patients.
CHAFA helps is a trusted partner with years of experience in combating healthcare fraud. With a varied range of services including coding, billing, compliance consulting, and management at your disposal, learn more about medical coding. Continuous progress and a commitment to perfection are the keys to success for medical coders in this ever-changing sector.

