
Clinical documentation is extremely essential in the ever-changing healthcare environment for accurate and thorough patient treatment. The quality of healthcare delivery, revenue cycle management, and regulatory compliance are all greatly impacted by proper documentation in addition to ensuring greater communication among healthcare professionals. Clinical Documentation Improvement (CDI) is a methodical strategy that aims to improve the precision, thoroughness, and specificity of medical records.
What is Clinical Documentation Improvement?
In a medical record, which serves as a repository for a person’s health information, clinical documentation is the data a person in charge of a patient’s medical treatment enters. A doctor, dentist, chiropractor, or other healthcare provider may have written the entries in the medical record.
The goal of clinical documentation improvement is to strengthen patient information documentation in order to foster better patient care, fair reimbursement, and regulatory compliance. To ensure that medical records accurately reflect the patients’ conditions and the treatment given, healthcare professionals, clinical documentation experts, coders, and other stakeholders collaborate.
A comprehensive and accurate clinical picture is captured by CDI, which reduces coding mistakes, enhances clinical judgment, and improves patient outcomes.
The Importance of CDI in Healthcare
1) Enhanced Patient Care
An accurate and thorough clinical record is used to keep track of a patient’s medical history, diagnosis, course of therapy, and results.
By using this data, healthcare professionals can decide on patient care with confidence, resulting in appropriate interventions and timely treatment schedules.
Additionally, better documentation makes it easier for healthcare providers to communicate effectively, which results in more coordinated and effective patient care.
2) Revenue Cycle Management
Coding mistakes can result from inaccurate or improper clinical documentation, which then affects the facility’s revenue cycle. In order to avoid claim denials or underpayments, proper documentation helps guarantee that the services rendered are appropriately classified and priced.
Thus, CDI helps healthcare organizations manage their revenue cycle more effectively and have more stable finances.
3) Compliance and Legal Protection
A crucial component of hospital operations is adherence to coding and billing laws.
By ensuring that medical records accurately represent the services actually provided, CDI lowers the possibility of fraudulent or non-compliant behavior. Furthermore, complete documentation improves the legal standing of healthcare facilities in the event of audits or legal issues.
Key Features of Effective CDI Programs
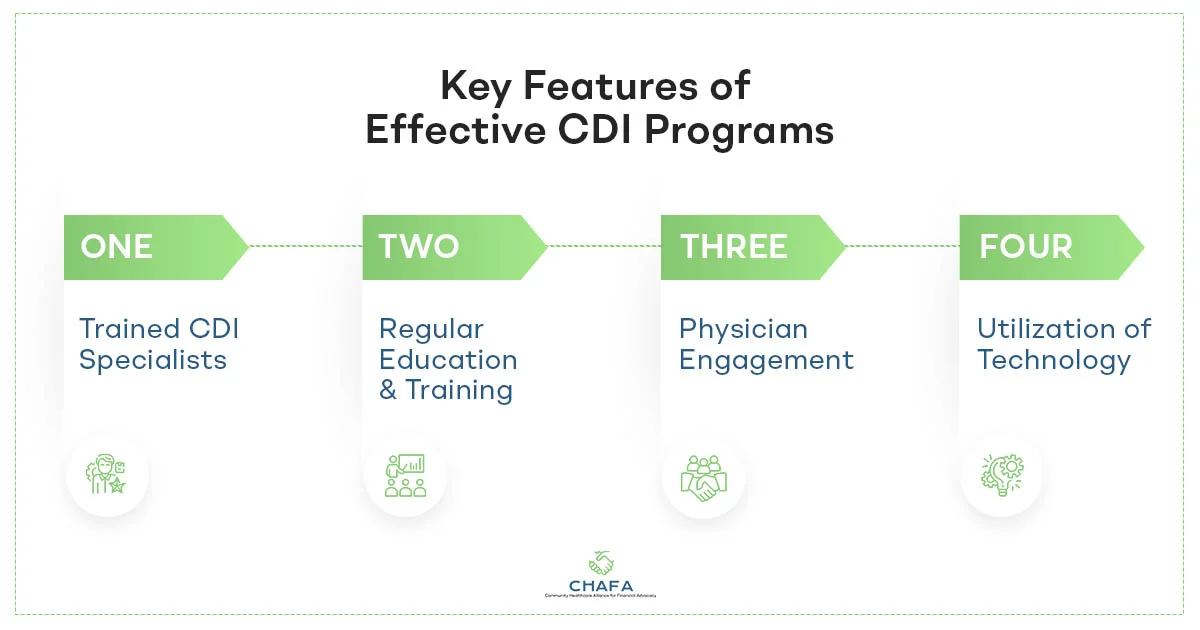
1) Trained CDI Specialists
Clinical Documentation Improvement programs rely on qualified specialists with in-depth knowledge of medical terminology, coding conventions (such as ICD-10 and CPT), and the specifics of various medical specializations. To gather precise and comprehensive clinical data, these specialists collaborate with doctors, nurses, and other healthcare professionals.
2) Regular Education and Training
For CDI specialists and other healthcare personnel, regular training and education is essential given the dynamic nature of healthcare rules and coding guidelines. The entire team stays up to date on the most recent industry changes and best practices through regular workshops, webinars, and seminars.
3) Physician Engagement
Physician involvement and support are essential for CDI programs to be successful. Doctors need to be aware of the value of correct documentation, as well as how it affects patient care and the organization’s financial stability. A culture of cooperation and progress can be established by promoting open communication and addressing concerns.
4) Utilization of Technology
The use of technology, such as Computer-Assisted Coding (CAC) and Natural Language Processing (NLP) tools, can be very advantageous for CDI programs. With the use of these technologies, clinical paperwork may be analyzed to spot any discrepancies and make suggestions for improvement.
CDI Implementation Strategies
- Conducting a CDI Readiness Assessment
Healthcare facilities should carry out a complete readiness assessment before launching a CDI programme. Examining the current documentation procedures, spotting any gaps, and comprehending the unique requirements of the organization are all part of this assessment.
- Setting Clear Objectives
Setting specific, attainable goals is essential to a CDI program’s success. Having clear objectives in mind helps in focusing efforts and evaluating performance, whether the goal is better patient outcomes, decreasing denials, or boosting reimbursement rates.
- Developing Comprehensive Policies and Guidelines
The documentation process is consistent and understandable thanks to a framework of CDI policies and guidelines that is well established. Best practices for documentation, coding standards, and protocols for dealing with questions and criticism should all be covered.
- Integrating CDI with Existing Workflows
Implementing CDI effectively necessitates seamless integration with current clinical workflows. As a result, disruptions are kept to a minimum and the CDI program is guaranteed to permeate the entire organization.
Impact of CDI on Patient Care and Healthcare Facilities
1) Improved Patient Outcomes
Healthcare professionals can better grasp a patient’s medical history, prior treatments, and current symptoms by having accurate and thorough documentation. Improved patient outcomes are the result of more accurate diagnoses and customized treatment programs.
2) Enhanced Communication and Collaboration
A strong CDI program promotes improved teamwork and communication among medical professionals. Healthcare professionals can readily exchange vital patient information, improving patient safety and facilitating care coordination, by ensuring uniform and unambiguous record keeping.
3) Financial Benefits for Healthcare Facilities
Effective CDI programs positively impact healthcare facilities’ financial health. By improving coding accuracy, reducing claim denials, and maximizing appropriate reimbursements, facilities can experience increased revenue and financial stability.
4) Reduced Legal and Compliance Risks
Proper documentation lowers the chance of compliance infractions and related legal issues thanks to CDI initiatives. In the event of audits or inquiries, a complete and compliant medical record can be used as legal justification.
By assuring accurate, thorough, and consistent documentation of patient information, clinical documentation improvement plays a crucial role in contemporary healthcare. Chafa has been a pioneer in the medical industry, ensuring accurate medical coding and healthcare compliance.

