Medical billing is an important part of the healthcare sector as it ensures that healthcare practitioners are properly reimbursed for the delivered services.
However, the complex nature of medical billing can result in errors that affect not just the revenue cycle but also patient satisfaction and overall practice efficiency.
In this comprehensive guide, we will look at the most common medical billing errors.
1) Duplicate Billing:
Duplicate billing happens when a healthcare professional files several claims for the same treatment.
This can occur unintentionally, such as when different departments within a healthcare facility file separate claims for the same patient interaction. Duplicate billing causes reimbursement delays and increases the likelihood of audits and legal implications.
Healthcare providers should establish sophisticated billing systems that detect duplicate claims before submission. Regular audits of billing records can also help detect and correct instances of duplicate billing.
2) Upcoding and Unbundling:
Upcoding involves billing for a higher-level service or procedure than what was performed. Meanwhile, unbundling refers to billing separately for components of a bundled service.
Both practices are deemed fraudulent and may result in significant fines, penalties, and criminal charges.
Healthcare professionals should ensure that services delivered are accurately documented and that codes are selected depending on the complexity and intensity of the patient interaction.
Coding and billing professionals should receive regular training and education to prevent upcoding and unbundling errors.
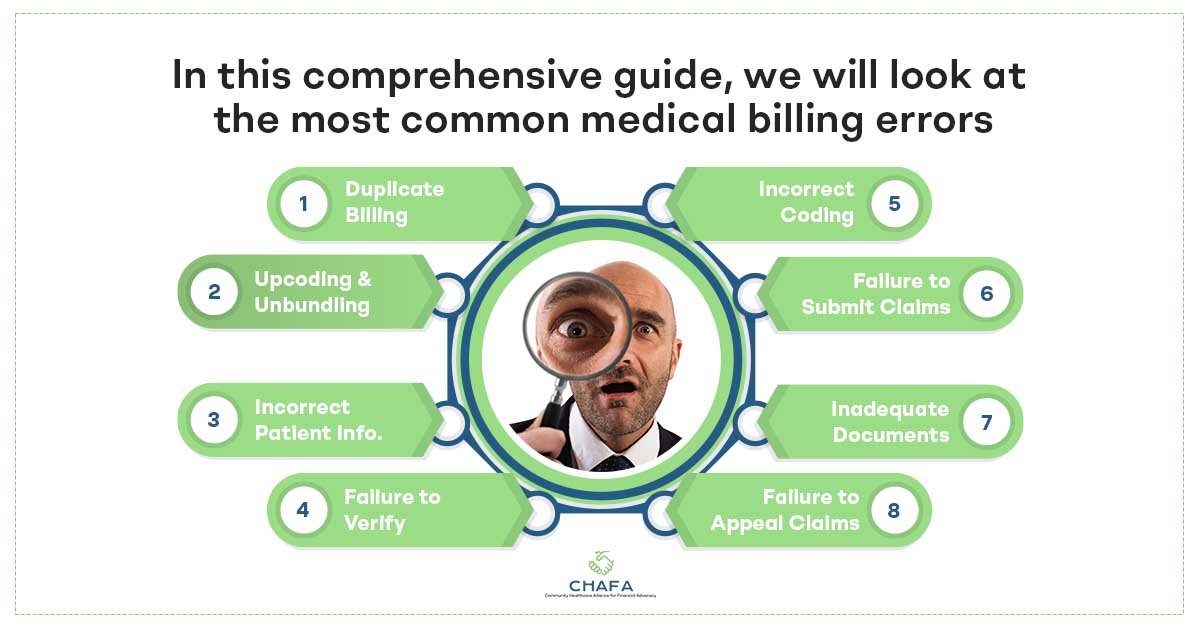
3) Incorrect Patient Information:
Incorrect patient information, such as misspelled names, wrong insurance information, or out-of-date demographic data, can result in claim denials and reimbursement delays.
Furthermore, it can cause misunderstanding and dissatisfaction among patients and healthcare providers.
To address this issue, healthcare providers should establish systems that validate patient information at the point of service and periodically update patient data.
Employees should be trained to confirm patient demographics and insurance information during the registration process to ensure accuracy.
4) Failure to Verify Insurance Coverage:
Failure to check a patient’s insurance coverage before providing services can lead to claim denials and the patient being responsible for the entire amount.
Healthcare providers must check insurance coverage eligibility, including coverage limitations, copayments, and deductibles, before providing services.
Automated eligibility verification solutions can speed up the process and lower the risk of human errors.
Furthermore, front-desk employees should be trained to collect and confirm insurance information during registration to avoid complications for patients and physicians.
5) Incorrect Coding:
Coding errors, such as the incorrect use of CPT (Current Procedural Terminology) and ICD (International Classification of Diseases) codes, can result in denied claims and delays.
Common coding errors include using out-of-date codes, mismatching diagnosis and procedure codes, and not providing enough evidence to back the codes billed.
Healthcare providers must invest in training for coding personnel to ensure appropriate code selection and documentation.
Regular chart audits can help in detecting coding problems and opportunities for improvement.
6) Failure to Submit Clean Claims:
Submitting clean claims that meet all the insurer guidelines is essential for receiving prompt reimbursement.
Errors like missing or incomplete information, a lack of supporting documentation, and noncompliance with requirements can all lead to claim rejections.
Healthcare providers should put in place mechanisms to ensure that claims are accurate and complete before they are submitted.
Automated claim scrubbing software can assist in discovering and rectify problems before sending claims to payers, lowering the risk of denials and delays.
7) Inadequate Documentation:
Lack of documentation to back up the services billed is a common reason for claim denials and audits.
Healthcare practitioners must ensure that all patient contacts are thoroughly and accurately documented, including chief complaints, history of current disease, physical examination findings, diagnostic test results, and treatment plans.
Implementing electronic health record (EHR) systems with built-in documentation templates and clinical decision support can help to shorten the documentation process and increase compliance with documentation requirements.
Regular provider education on proper documentation methods is also required to reduce the likelihood of errors. Having a medical billing specialist can help smoothen this process.
8) Failure to Appeal Denied Claims:
Denials are an inevitable part of the medical billing process, but failing to appeal denied claims can result in lost revenue. Healthcare providers should have robust processes in place to identify and appeal denied claims promptly.
Designating staff members to manage the appeals process and track claim status can help expedite the resolution of denied claims.
Additionally, analyzing denial trends and addressing root causes can help prevent future denials and improve overall revenue cycle performance.
Conclusion:
Effective medical billing is essential for the financial health and sustainability of healthcare practices.
By identifying and addressing common billing errors, healthcare providers can improve revenue cycle management, enhance patient satisfaction, and optimize practice efficiency.
The expert team at CHAFA helps you implement proactive measures to mitigate the risk of billing errors and ensure timely reimbursement.

